How lab-grown “lungs” are helping fight infectious diseases
VIDO scientists have developed tiny, lab-grown “mini lungs” that mimic real human lungs, giving researchers a powerful new way to study how viruses infect us and accelerate the development of vaccines and treatments.
By Caitlin GillWhat if scientists could build a realistic model of the human lung, not full-sized, but grown in the lab from living cells? Why would they do this? VIDO scientists based at the University of Saskatchewan have been exploring exactly that, and their work shows that these small, 3D structures referred to as “organoids” behave much like real lungs, giving scientists a powerful new way to study how viruses infect us.
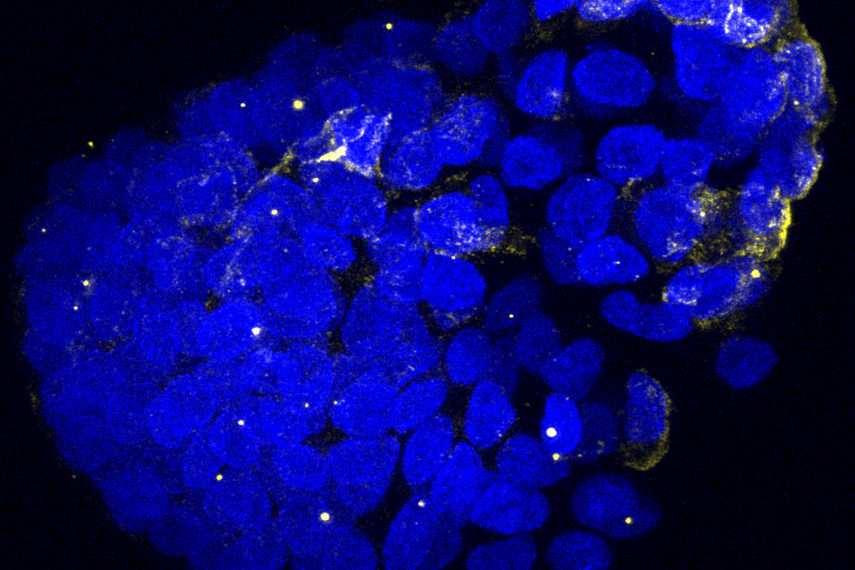
Organoids aren’t actual full-sized lungs that breathe. Instead, they are ‘mini lungs’, about the size of a grain of salt, derived from stem cells or human tissue samples that can grow into the kinds of tissues found in our body. These little clusters of cells can look and act a lot like real lungs, which makes them a powerful tool for science.
“Developing miniature lung models allows us to study emerging viruses in ways that were not mainstream before,” said Dr. Volker Gerdts, VIDO director and CEO. “These advances strengthen Canada’s role in pandemic preparedness and accelerate the discovery of vaccines and treatments.”
So why develop organoids in the first place? The answer has a lot to do with how viruses like MERS-CoV (the virus that causes Middle East Respiratory Syndrome) and SARS-CoV-2 (the virus that causes COVID-19) infect our bodies.
Typically, scientists study viruses in flat sheets of cells on plastic dishes (referred to as ‘in-vitro’). But the human body isn’t flat and lungs are complex organs with many different cell types; some that absorb oxygen, some that create mucus, and others that act like security guards fighting off germs. A flat dish can’t capture that complexity, which means scientists may miss important details about how viruses attack us.
That’s where 3D mini lungs come in.
In a recent study, VIDO scientists used lung organoids they made in the lab to study how MERS-CoV and SARS-CoV-2 infect human lungs. What they found was eye-opening. The two viruses didn’t just spread randomly. They infected specific types of lung cells. Some cells were especially vulnerable, while others were more resistant. Understanding these differences helps explain why these viruses make people sick in different ways.
For example, MERS-CoV has long been known to cause very serious illness, often with a high case fatality rate (estimated at 33%). SARS-CoV-2, while deadly for many, often causes mild or even symptom-free infections. By seeing exactly which lung cells the viruses infect, scientists can piece together why their impacts aren’t the same.
"It is so exciting that lung organoids could help test future antiviral therapies by identifying the sites of virus infection," said Dr. Arinjay Banerjee, VIDO scientist. "Imagine being able to try out a new antiviral drug on a 'mini lung' before ever giving it to a patient. This will enable scientists to see whether the drug works, what cells it protects, and even whether there are side effects."
This kind of research could also prepare us for the next pandemic. If a new respiratory virus shows up tomorrow, scientists could grow mini lungs in the lab and quickly learn what parts of the lung it targets, and test a multitude of drugs simultaneously to determine how best to fight it. That’s a huge step forward.
“Organoids provide us with a safe and powerful system to test how new viruses behave, and how potential therapies might work, before moving to pre-clinical studies or human trials,” said Dr. Neeraj Dhar, VIDO scientist. “This technology is an important bridge between the lab and real-world solutions.”
Scientists aren’t 3D printing full-sized human lungs just yet. But these tiny, lab-grown versions are opening a whole new window into how our bodies work and helping scientists tackle some of the biggest challenges in global health.
Want to see the science behind it? Read the paper → https://journals.asm.org/doi/10.1128/jvi.01098-25

